The Lymph Info Trust exists to improve the quality of life of anyone in New Zealand who has a lymphatic condition. We aim to do this through education and raising awareness.
We empower New Zealanders who are living with:
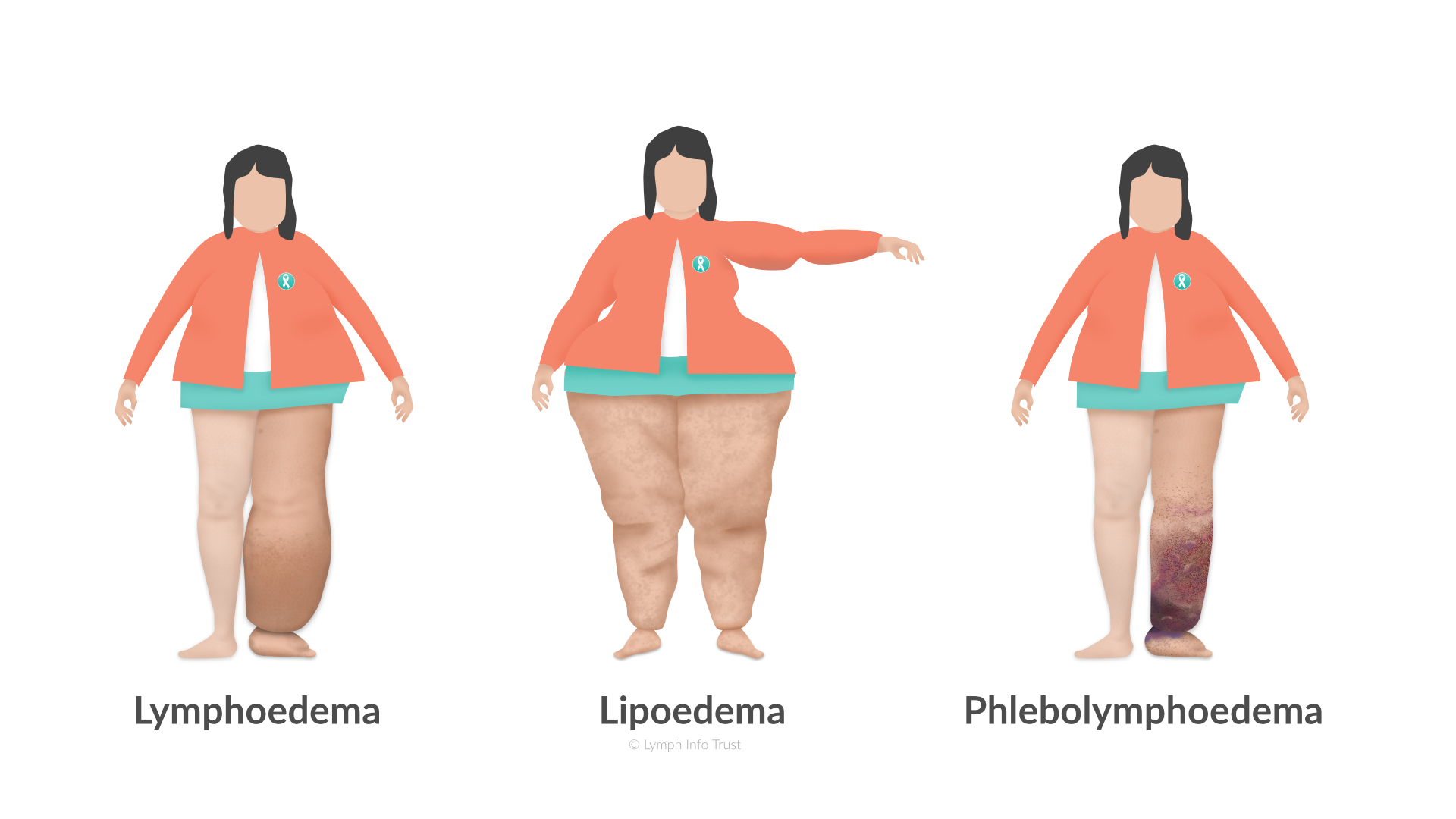
- lymphoedema
- lipoedema, and
- phlebolymphoedema.
We provide understandable information, education and resources. We do this to help your understanding of oedema and its treatments.
Swelling (Oedema / Edema)
Oedema is more related to visible symptoms (swelling) and primarily associated with lymphoedema. It may also be known as:
- fluid retention
- dropsy, or
- hydropsy.
Symptoms and treatment will vary depending on the cause of the swelling.
Swollen Ankles and Feet During Pregnancy
In late pregnancy, the weight of the uterus can press down on the veins of the pelvis resulting in swollen legs and ankles. This swelling should clear up after giving birth. Even though it is not a cause for concern, please discuss any swelling with your doctor or lead maternity carer (midwife).
Lymphoedema (Chronic Oedema)
 Lymphoedema is a condition where damaged lymphatic vessels cause a failure of the lymphatic drainage system. This swelling in turn leads to chronic swelling of a limb (arm or leg), or other part of the body.
Lymphoedema is a condition where damaged lymphatic vessels cause a failure of the lymphatic drainage system. This swelling in turn leads to chronic swelling of a limb (arm or leg), or other part of the body.
Primary Lymphoedema
Primary lymphoedema is congenital. That is, some people are born with this condition. There is a strong link between genetics, family history and hormonal milestones. Symptoms typically develop during the teenage years.
Secondary Lymphoedema
Secondary lymphoedema occurs when the lymphatic system is damaged. The lymphatic system can be damaged as a result of:
- injury
- surgery
- radiation therapy
- infection, or
- a blockage caused by a tumour.
Lipoedema
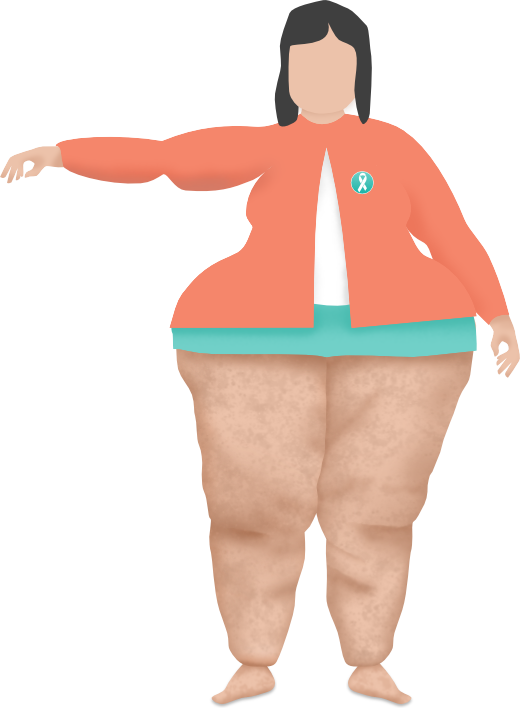
Lipoedema is a condition where fat (lipids) are deposited over the lower part of the body; from the hips to the ankles of both legs, but generally not the waist, nor the feet.
Phlebolymphoedema
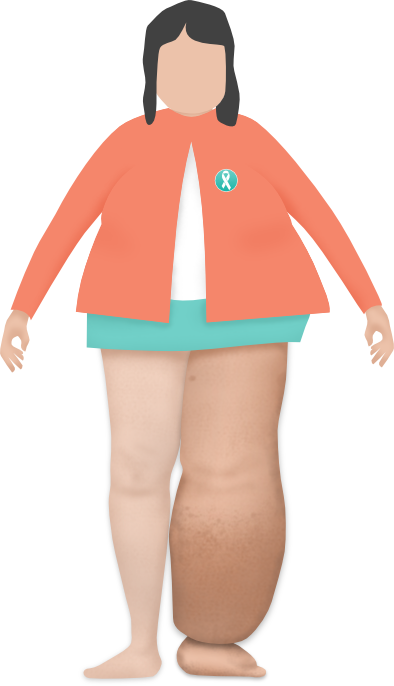
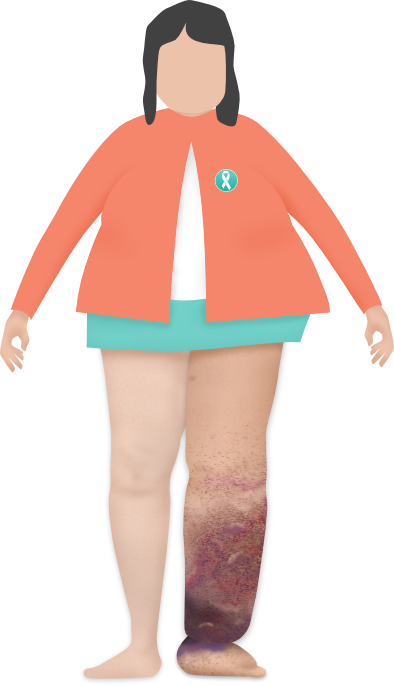 Phlebolymphoedema is a secondary lymphoedema.
Phlebolymphoedema is a secondary lymphoedema.
Phlebolymphoedema is the accumulation of excess intercellular/interstitial fluid in the legs and feet, resulting from the combined conditions of phlebodoema and lymphoedema.
Phlebogenic oedema is called phleboedema.
Lymphogenic oedema is called lymphoedema.
To put it simply, phleboedema + lymphoedema = phlebolymphoedema.
Phlebolymphoedema is the inevitable failure of the:
- venous circulation system, and
This is an interconnected system of veins and sinuses. - lymphatic circulation system.
This is the system that circulates a clear fluid called 'lymph' back into your bloodstream.
Both systems work together to remove used blood from tissue. If one system fails, the other will also fail.
Lymphatic Filiarisis
Lymphatic Filiarisis, also known as Elephantiasis, is a secondary lymphoedema. It is common around the tropical and sub-tropical regions. The cause of Lymphatic Filiarisis is a mosquito-born parasitic worm. This worm is not present in New Zealand. It can affect both men and women, and the symptoms include swelling of the scrotum, legs or breasts.
Medication-Induced Oedema
Some medicines can cause oedema. Talk to your doctor about the possible side effects of any medications you are on. The following medications are known to contribute to oedema.
- Medications with high levels of sodium and sodium bicarbonate, e.g., antibiotics
These can cause sodium overload / retention. - NSAIDs, anti-hypertensives, and anticancer drugs
These drugs may exacerbate any pre-existing renal dysfunction in patients and cause oedema. - Calcium antagonists, insulin, etc
These increase vascular permeability and contribute to hyper-permeability.